The healthcare billing audit process is an organized procedure that reviews and examines medical data and documents to ensure accuracy. A medical billing audit investigates the effectiveness and reliability of medical documentation within a provider’s practices. The process includes thorough check-ups of all health records and the billing data submitted by payors.
What is a Billing Audit Process?
A medical billing audit is all about combing through all present data and records to monitor, identify, and correct inaccurate, incomplete, or inappropriate billing practices. Healthcare billing audits identify compliance issues that can impact the bottom line or even result in penalties with Medicare if your practice is credentialed.
Importance of Medical Billing Audit for Your Practice
Audits are critical for the success of any healthcare practice. Medical audits pinpoint areas where improvements are needed in services or procedures as a healthcare provider. Furthermore, a healthcare billing audit helps ensure efficient and accurate documentation of medical records.
But how do we ensure healthcare compliance for a medical billing audit? – Check out our:
Billing Audit Process Checklist
To stay on top of your healthcare billing audit, follow this checklist:

Step 1: Define Scope and Resources
- Identify the scope of your billing audit and determine the resources, including staffing, required for execution.
- Designate the task to a team member or consider third-party consultation services to conduct the audit.
- Factor in audit tactics, and select several charts per provider and payer to review data versus documentation.
- Document everything and circulate a complete audit plan among your team.
Note: Preventing coding and billing errors can still be challenging, even with extensive knowledge of providers’ services and linked diagnoses.
Step 2: Review Billing Reports
- Review all billing reports to categorize risk areas and identify troubling trends.
- Compare irregularities with past performances to spot patterns.
- Analyze physician service frequency versus peers over a set period, including running E&M frequency reports.
- Generate a report detailing how CPT codes are reimbursed.
Step 3: Set Targets and Make Improvements
- After gathering information, set specific improvement targets.
- Persuade payors to pay contracted rates accurately and timely.
- Follow up diligently and develop a plan for dealing with delinquent payers.
- Address internal issues identified in the audit, including training for providers and staff.
Step 4: Make Audits a Routine Practice
- Incorporate billing audits into regular procedures to simplify future audits.
- Run frequent reports and monitor net collections consistently.
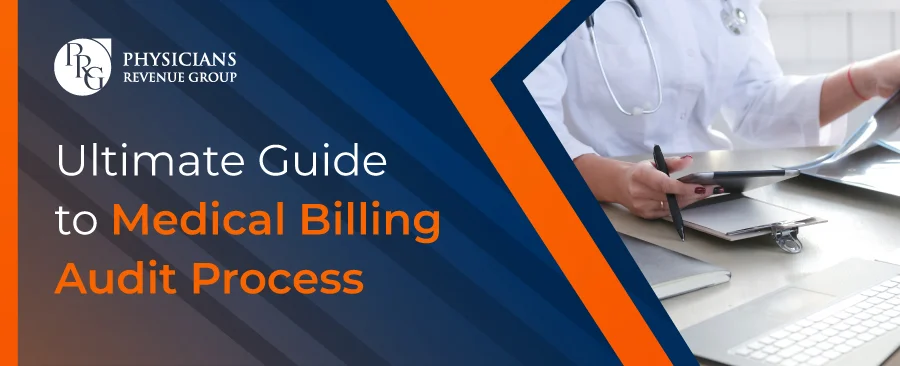
Advantages of Billing Audit Process


Billing audits offer numerous benefits and should be a continuous practice within your healthcare organization:
- Boost Profitability: Conducting audits can improve overall revenue.
- Identify Errors: Locate incomplete, inaccurate, or inappropriate billing practices that could cost your practice.
- Catch Unrecorded Charges: Unnecessary or unrecorded charges for services or items can be corrected.
- Support Coding Staff: Helps coding staff identify and fix errors before they are caught by insurers or government agencies.
- Improve Documentation: Better medical record documentation increases reimbursements for services rendered.
- Standardize Processes: Establishes a standard workflow for administrative staff, reducing stress and mistakes.
- Protect Against Fraud & Compliance Issues: Ensures compliance and helps prevent fraudulent claims.
- Medicare Compliance: Essential for services billed through Medicare.
- ICD-10 & EHR Verification: Helps ensure readiness and meaningful use of electronic health records.
- Best S&P 500 Skyrockets as Nvidia Ignites Market Surge

- How Proper Documentation Can Save Time and Money

- FDA Announces Recall on Powerful M&M’s Products in 20 States

- best Maximizing Returns: Real Estate Investment Secrets

- Best Alphabet’s Massive 2026 AI Spending Stuns Wall Street

- Ultimate Guide to Best Medical Billing Audit Process
Final Thoughts
A consistent and systematic billing audit process benefits medical practices at multiple levels. An expert team should be dedicated to your practice to avoid drawbacks and improve overall revenue cycle management (RCM).
One effective strategy to reduce the likelihood of coding or billing errors while boosting RCM is to outsource your medical billing audit services. A third-party billing audit company, such as Physicians Revenue Group, Inc., with:
- The right resources
- Detailed practice management knowledge
- Operational capacity
- Targeted billing audit tools
…can manage all claims and help identify audit-inducing issues before they arise.
Frequently Asked Questions
#MedicalBillingAudit #BillingAuditProcess #HealthcareCompliance #Carrerbook #Anslation #MedicalCoding #RevenueCycleManagement #RCM #HealthcareBilling #MedicalAudit #HealthcareDocumentation #MedicalBillingServices